If left untreated, Biliary Atresia progression to end-stage cirrhosis usually occurs within one year
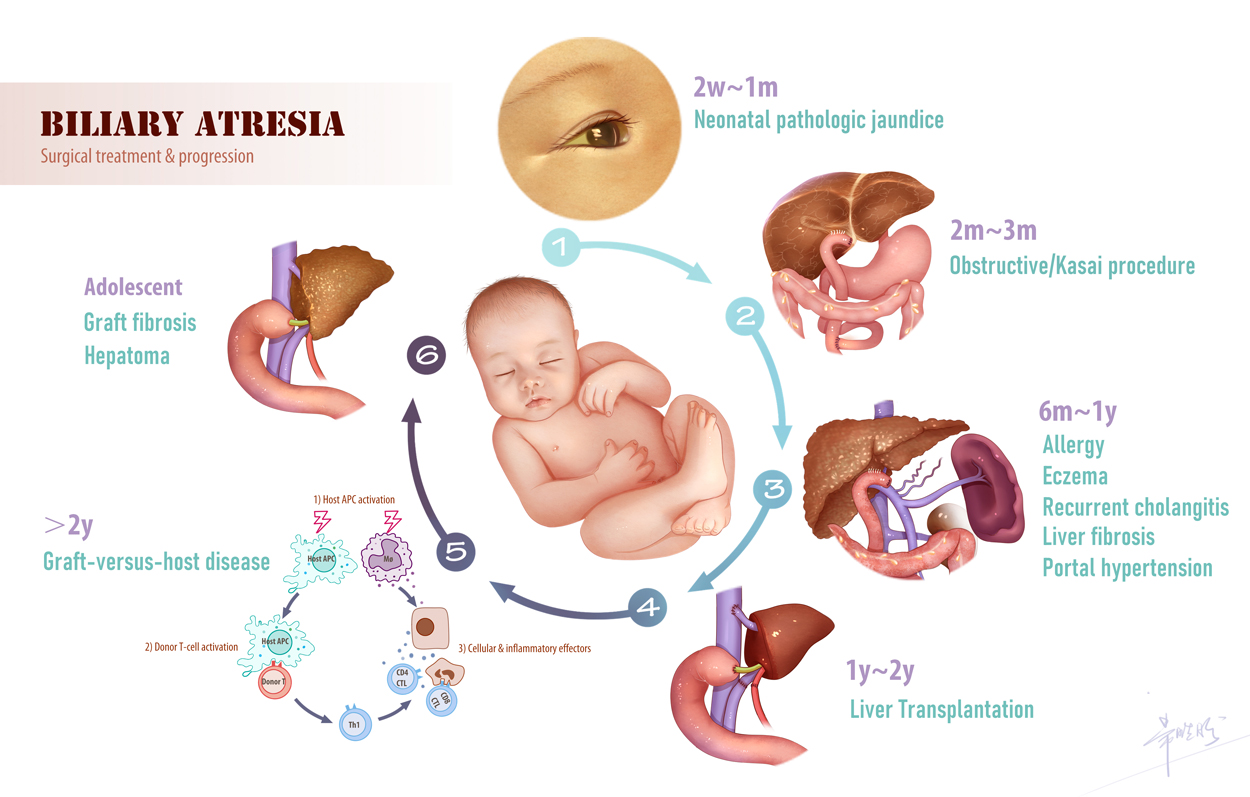
Biliary Atresia (BA) affects one in every 5,000-18,000 newborns. Perinatal infection is a significant trigger, which can cause obstruction of the extrahepatic bile duct and rapid liver failure. Surgical removal of the duct remnants followed by hepatoportoenterostomy (Kasai’s procedure) is required after diagnosis. If left untreated, Biliary Atresia progression to end-stage cirrhosis usually occurs within one year. Following the Kasai’s operation, approximately 50% of the Biliary Atresia patients will require liver transplantation within the first 2 years of life, while the remainder children surviving with the native livers will suffer long-term complications including repeated cholangitis, portal hypertension, esophageal variceal bleeding, and hepatic osteodystrophy.
At Pediatric Immunity and Healthcare, we have been developing biomarkers and therapies that may improve the outcome of infants with Biliary Atresia. These biomarkers employ immunological and biochemical changes associated with perinatal infection. Our aim is to decrease disease occurrence and improve clinical outcomes via early diagnosis and therapy.
Yuxia Zhang
12 September 2021